The following text is a direct transcript from “Prevention and Treatment of Pressure Ulcers: Short Version of Guidelines 2019”.
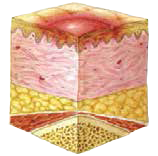
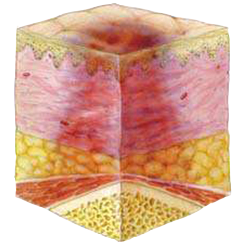
Category I – Redness that does not reduce on pressure
Intact skin with redness in a clearly defined area, usually above a bone protuberance, that does not reduce on pressure. Dark, pigmented skin might not show this sign, though the colour is different from the surrounding areas of skin. The area may be painful, solid or soft, and warmer or colder than other areas of skin. Category I pressure ulcers may be difficult to detect in people with dark skin tones. Category I pressure ulcers may be a sign that the patient is in the risk zone for developing deeper pressure ulcers (1).