References
(1) European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The international Guideline. Emily Haesler (Ed.). EPUAP/NPIAP/PPPIA: 2019
(2) KOSIAK M. (1959). Etiology and pathology of ischemic ulcers. Archives of physical medicine and rehabilitation, 40(2), 62–69.
Witkowski, J. A., & Parish, L. C. (1982). The decubitus ulcer. International journal of dermatology, 21(5), 259. https://doi.org/10.1111/j.1365-4362.1982.tb02092.x
(3) Witkowski, J. A., & Parish, L. C. (1982). The decubitus ulcer. International journal of dermatology, 21(5), 259. https://doi.org/10.1111/j.1365-4362.1982.tb02092.x
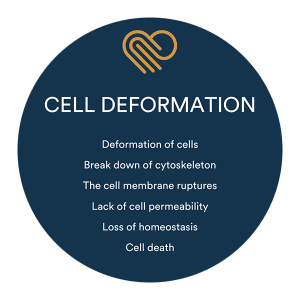
(4) Leopold, E., & Gefen, A. (2013). Changes in permeability of the plasma membrane of myoblasts to fluorescent dyes with different molecular masses under sustained uniaxial stretching. Medical engineering & physics, 35(5), 601–607.
(5) Gefen, A., Brienza, D. M., Cuddigan, J., Haesler, E., & Kottner, J. (2022). Our contemporary understanding of the aetiology of pressure ulcers/pressure injuries. International wound journal, 19(3), 692–704. https://doi.org/10.1111/iwj.13667